Pain specialist reports that although women experience more pain, doctors’ approach is often inadequate and disrespectful
A survey by the Brazilian Society for the Study of Pain (SBED) showed that women are more frequent victims of chronic pain than men. This is because they tend to have more neck and shoulder pain, abdominal pain, tension-type headaches, migraines after puberty, TMJ (temporomandibular joint) disorders, and others.
html[data-range=”xlarge”] figure image img.img-8901060b431d445c897a5ca1b2e0f952h1wvujnj { width: 774px; height: 463px; }HTML[data-range=”large”] figure image img.img-8901060b431d445c897a5ca1b2e0f952h1wvujnj { width: 548px; height: 328px; }HTML[data-range=”small”] image figure img.img-8901060b431d445c897a5ca1b2e0f952h1wvujnj, html[data-range=”medium”] figure image img.img-8901060b431d445c897a5ca1b2e0f952h1wvujnj { width: 564px; height: 337px; }
To give you an idea, the ratio of women to men in the prevalence of painful conditions is on the order of 1.5 to 1 in low back, shoulder and knee pain. It’s 2 to 1 in orofacial pain. 2.5 to 1 in migraine (throbbing pain affecting the side of the head). And 4 to 1 in fibromyalgia, a chronic disease whose main symptom is constant pain throughout the body.
According to the SBED, there are several specific pain syndromes for women. In particular it is dysmenorrhea (pelvic pain that appears on the first day of the menstrual period and disappears when the flow ceases). It affects between 49% and 90% of women and is very painful in up to 15% of cases.
In addition, there are other pain syndromes that particularly affect women. This is the case with chronic pelvic pain, chronic vulvar pain, low back and pelvic pain during pregnancy, and pain during childbirth.
Why do women feel more pain?
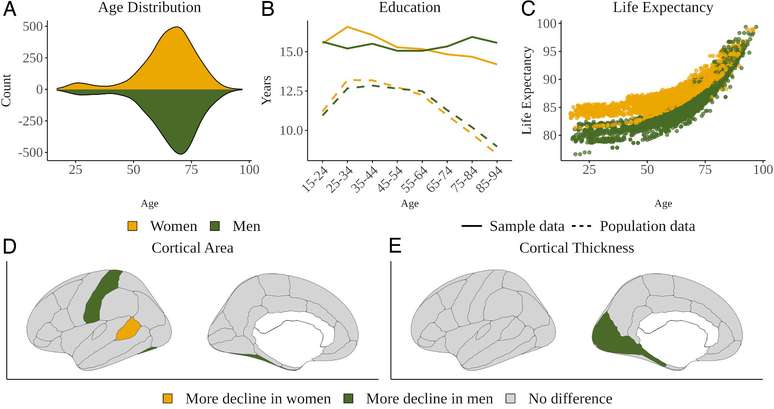
Pain specialist Dr. Amelie Falconi explains that several studies have consistently shown gender differences in chronic pain. Such as, for example, the perception, description and expression of discomfort, the use of coping strategies and the benefits of different treatments. There are compelling findings that biological differences contribute to the observed differences between the sexes.
She says there are several reasons why women feel more pain than men. Genetic factors, for example, including hormonal factors, act as sex-specific pain mediators. “Studies show that a woman’s response is influenced by her menstrual cycle, pregnancy, and can be influenced by oral contraceptive use as well,” Amelie adds.
Estrogen, a hormone essential for female reproductive function, for example, when its levels increase or decrease in the female body, is responsible for increasing cellular excitation. More specifically, estrogen fluctuations can increase neural growth factor expression, the number of excitatory synapses in the hippocampus, glutamate binding to the NMDA receptor, and excitatory postsynaptic potentials.
minimal pain
For the specialist, it is worth discussing the relationship of women with pain. The aim is to show how, despite being more susceptible to this physical suffering than men, they are still victims of many prejudices regarding diagnosis and treatment.
Although the discomfort is more widespread and more intense in women, Dr. Amelie points out that women tend to minimize their painful ailments from society more often than men. “Many times I have heard, even from specialized doctors, that a certain patient’s pain was ‘fresh’ or psychological and that the patient’s intention was to attract attention, both from her husband and children, and from other people “, he reports.
The doctor comments that it is common even in these professional situations to judge the patient’s life to minimize her complaints. “I’ve heard unnecessary comments from healthcare professionals about patient photos on social networks. The fact that a patient travels on the weekend doesn’t take away from her the credit for the pain she’s in,” she says. You also specify that the patient’s activities outside the study should not interfere with the evaluation of the treating physician.
Amelie also says that these types of comments and judgments do occur among people in the social circle of chronic pain sufferers. “I often hear comments that minimize the pain of patients. Even having patients do their hair or put on makeup have already been talking points about the veracity of pain. The public needs to understand that patients with chronic pain get used to wearing their their routine activities even in pain,” points out the doctor.
Science has already confirmed this
The specialist points out that the difference in the approach of the patient with chronic pain compared to men has already been demonstrated, including by a scientific study. He reports that a review article brought up 77 articles in the literature dealing with men and women with pain, gender norms, and gender bias in treating the condition.
“The survey observed a paradox. Although chronic pain is more prevalent and more intense in women, women’s relationships are taken less seriously, their pain is discounted as psychic or non-existent, and their treatment is less adequate than that given to men”. she reports. As a result of this disdain, according to the review article, women are often medicated with more antidepressants and fewer pain relievers.
For the researchers, this lack of attention from professionals to female patient complaints is an expression of hegemonic masculinity and anormativity in health care. Dr. Amelie agrees with the conclusion. “This article exposes the issue of machismo in pain care. If chronic pain is known to affect more women, why when they come to the office and complain about pain, are they immediately labeled as emotionally weak?” she asks.
Source: Terra
Ben Stock is a lifestyle journalist and author at Gossipify. He writes about topics such as health, wellness, travel, food and home decor. He provides practical advice and inspiration to improve well-being, keeps readers up to date with latest lifestyle news and trends, known for his engaging writing style, in-depth analysis and unique perspectives.




![Tomorrow belongs to us: What awaits you in the episodes of 2052 and 2053 on October 15, 2025 [SPOILERS] Tomorrow belongs to us: What awaits you in the episodes of 2052 and 2053 on October 15, 2025 [SPOILERS]](https://fr.web.img6.acsta.net/img/39/95/3995a2d00abbf3c01161818d01a95388.jpg)



