These benign lumps in the uterus are quite common, but sometimes they are very destructive.
About 80% of women of childbearing age have fibroids, benign nodules that form in the muscle cells of the wall of the uterus, the myometrium. Most of them do not cause discomfort or require treatment. But for many women, the condition can affect their quality of life or even lead to serious complications.
“If we compared the uterus to a room, we could say that the endometrium is the paint on the wall, while the myometrium is the brick”, comments gynecologist Thiers Soares, president of the Brazilian Society of Minimally Invasive and Robotic Surgery (Sobracil), a Rio de Janeiro, and doctor at the Pedro Ernesto University Hospital, of the State University of Rio de Janeiro (UERJ).
The curious thing, according to him, is that, contrary to what many imagine, the fibroid is not a mass of cells, but rather a cell that, for some reason, begins to grow too much.
Symptoms
See the main symptoms of uterine fibroids, also called fibroids:
– Heavy bleeding during menstruation and sometimes between menstrual periods, which can cause anemia.
– Pain and cramps.
– Compression of the organs around the uterus, such as the bladder and bowel, which may increase the urgency to urinate or cause constipation.
– Depending on the location and volume of the fibroid, it may be difficult to get pregnant and increase the risk of miscarriage.
Classification
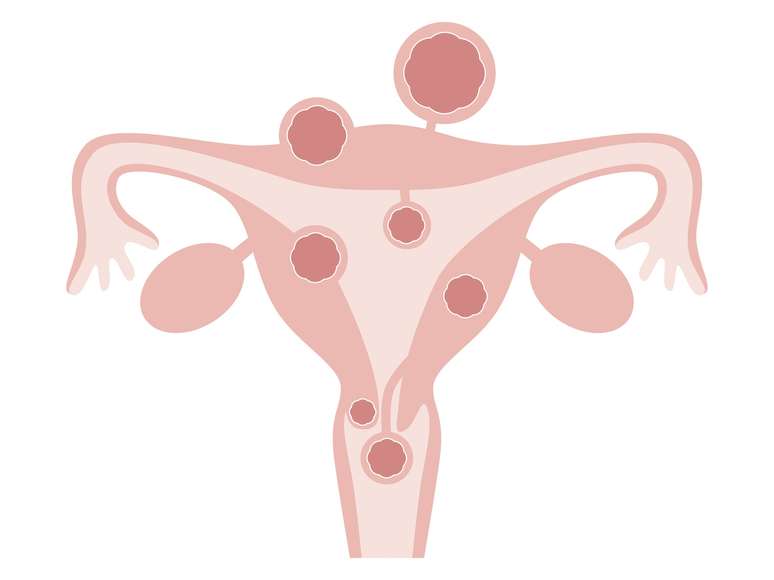
Fibroids can be classified based on where they develop:
Subserosal: on the external surface of the uterus;
Intramural: developed and localized in the walls of the uterus;
Submucosa: growth occurs in the internal part of the uterine cavity.
Fibroids and fertility
“Submucosal fibroids are the ones that most hinder fertility,” comments gynecologist Thiers Soares, president of the Brazilian Society of Minimally Invasive and Robotic Surgery (Sobracil), in Rio de Janeiro, and doctor of the Pedro Ernesto University Hospital, of the State University of Rio de Janeiro (UERJ). Subserous ones do not tend to hinder those who want to have children. “Intramural treatment can reduce the risk of pregnancy if the cavity swells,” he adds.
Risk factors
What exactly causes fibroids to grow is still not entirely clear. But factors that increase the risk:
– genetics (having relatives with a history of fibroids increases the likelihood of having the condition)
– age (most common after 30 years)
– race/ethnicity (more common in blacks than whites)
– never been pregnant
– obesity and overweight
– hypertension (high blood pressure)
A recent study, published in the scientific journal BMJ openhighlighted a relationship between a sedentary lifestyle and a greater tendency to have fibroids. The work involved 6,600 people, aged between 30 and 55. Of the total, 562 had fibroids.
Participants who reported spending six or more hours of free time without moving were twice as likely to have fibroids than those who reported less than two hours.
This difference was even more significant for perimenopausal women: Those in the most sedentary group were five times more likely to have fibroids than those with a shorter sedentary period. But further studies are still needed to confirm the association.
The gynecologist says other research also suggests a relationship between fibroids and low levels of vitamin D and soy consumption. But he believes that genetics is still the most important risk factor, which can determine the presence of these benign tumors even when no other factors are present.
Fibroids and estrogens
What is clear is that high levels of estrogen fuel the growth of fibroids, which also explains, for example, why obesity is a risk factor: adipose tissue increases this hormone. Also for this reason, after menopause the volume of fibroids tends to decrease.
Treatments
Despite the relationship between fibroids and estrogen, the use of hormonal contraceptives may be indicated to help control symptoms, such as bleeding and pain, as well as prevent their growth. You can also use methods that contain only progestin, such as the pill and hormonal IUD.
Anti-inflammatories and analgesics can relieve pain, in case of anemia iron supplementation may be necessary.
In case of compression of the surrounding organs or difficulty getting pregnant, surgical removal of the fibroids (myomectomy) is recommended. Today there are minimally invasive modalities, such as radiofrequency (a needle that emits heat to destroy part of the fibroid) and hysteroscopy (a camera with a handle fragments the fibroid and removes it).
Depending on the size and location, procedures can be performed vaginally (without cuts), laparoscopy (with a few small incisions), or laparotomy, in which an incision similar to that of a cesarean section is made.
Robotic surgery is also an option, although it is even more present in private hospitals: “It brings less pain, less chance of thrombosis and can allow the removal of a greater number of fibroids,” reports the doctor.
Removal of the uterus (hysterectomy) should only be considered when the patient does not want to become pregnant or has already had children. “It is very important to respect the desire for preservation of the uterus,” she emphasizes. Unfortunately, according to him, some doctors do not take this aspect into account and do not even propose another option. It is worth noting that hysterectomy may slightly increase the risk of vaginal prolapse or urinary incontinence in the future.
Another minimally invasive treatment option is fibroid embolization, which involves introducing a catheter through the groin into the uterine artery and delivering agents into the vessels that feed the fibroids. Approximately 90% of patients report an improvement in symptoms.
In short, it is essential that each case, as well as the pros and cons of each treatment, are well discussed between doctor and patient.
Source: Terra
Ben Stock is a lifestyle journalist and author at Gossipify. He writes about topics such as health, wellness, travel, food and home decor. He provides practical advice and inspiration to improve well-being, keeps readers up to date with latest lifestyle news and trends, known for his engaging writing style, in-depth analysis and unique perspectives.