The virus, endemic to West and Central Africa, is now present in 65 countries.

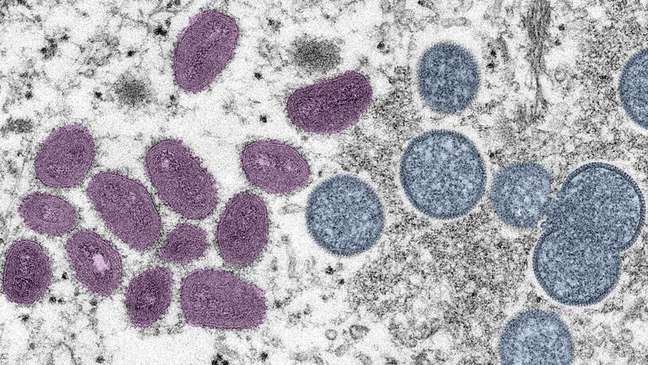
It is a known disease and humanity has fought against it in the past, but infections are on the rise around the world and governments have so far been unable to contain it. Monkeypox, a zoonotic condition endemic to West and Central Africa, is now present in 65 countries, unprecedented.
Positive cases of the virus, according to the US Centers for Disease Control and Prevention (CDC), have been 11,068 worldwide as of Wednesday, July 13.
As the Pan American Health Organization (PAHO) said this week, the trend is that infections will continue to rise in the coming weeks.
According to experts consulted by BBC News Mundo, the BBC’s Spanish service, a combination of factors, most notably the fact that monkeypox has not yet been declared an international health emergency, explains this explosion of cases.

Despite its rapid spread, and contrary to what some independent researchers claim, APHO director Carissa Etenga said the risk posed by monkeypox “is moderate” due to the low mortality relative to the number of reported cases.
However, in an interview with journalists, Sylvain Alighieri, APHO’s director of health emergencies, called the situation “worrying”.
“In many countries in the region for which we have well-characterized information, the proportion of cases with no travel history increases with each epidemiological week, which highlights our concern that more sustained transmission will take hold,” Alighieri said.
While most people recover from the virus, which causes skin rashes and flu-like symptoms like fever and headache, there are concerns that it may become endemic outside of Africa.
Monkeypox was first reported in 1970. There are approved antivirals and vaccines against the disease, as well as tests to detect the virus and sufficient knowledge of how it spreads.
So why are cases on the rise?

WHO response
For doctor Kavita Patel, a public health policy specialist and former White House advisor during Barack Obama’s presidency, one explanation for this is the fact that the World Health Organization (WHO) did not declare monkeypox. an international health emergency.
Without consensus among its members, the institution’s Emergency Committee realized last June that, precisely because of the low mortality, the disease did not represent a greater risk, although it should be monitored closely.
Patel argues that this decision affects global cooperation to tackle the virus, such as equitable distribution of existing vaccines among at-risk groups, which would help contain the increase in cases.
“The lack of an emergency declaration leaves us without global coordination, without the necessary money and resources being established,” he said.
The WHO action, which will be re-evaluated by the body next week, could make citizens understand the risk that the disease can carry, says Carlos Rodríguez Díaz, professor of public health at George Washington University in the United States.

“When a health emergency is declared, it is an indicator that the response needs to be intensified,” he said. “There is no good distribution of reliable and available information to the populations who need it most,” she added.
When the disease spread
The first cases of monkeypox, a disease that spreads most effectively through physical contact, were detected a few months ago outside of Africa among men who have sex with men. This has made gays a risk group.
And, according to Alighieri of PAHO, the cases in this community continue to grow due to the coincidence that in the months of June and July Gay Pride Month is celebrated in several countries, events that bring together millions of people.
Kavita Patel, in turn, recalled the importance of emphasizing that smallpox is not a disease that affects only homosexual men.
Conversely, linking this virus to sexual orientation could cause an increase in cases because other groups would also not know they are at risk.
“It reminds me of the early days of HIV, when we identified it as a disease related to gay people … and we are still dealing with the consequences around the world,” he said.
Problems detecting the virus
Globally, Patel continues, tests to detect the virus are not very accessible to the population, focusing on some laboratories and academic centers but not in community clinics and other direct care facilities.
“This leaves us exposed to people who unknowingly have monkeypox and can pass the disease on to other people. Even if they have a rash and some symptoms, they might think it’s a cold because the symptoms are sometimes similar,” he said. commented.

“In Central America, for example, people seek help from their neighborhood health workers. And now these providers have virtually zero access to testing,” he said.
In fact, PAHO data indicates that, of the more than 1,400 positive cases in the American continent, only one has been recorded in Central America.
“We don’t even know the real number of cases in the world,” says the expert.
The vaccine problem
Currently, there are two effective monkeypox vaccines. One, called Jynneos, is newly manufactured and has only been approved in the United States and Canada.
The other is the ACAM 2000 vaccine, used against traditional smallpox.
But, according to Professor Carlos Rodríguez-Díaz, the reserves of both are limited and, at the moment, international health organizations and governments cannot carry out mass vaccinations, which leaves the population unprotected.

The New York Times reported in early July that the Danish company that makes Jynneos would ship 2 million doses to the United States, but that won’t happen until the end of 2022. And it only has the capacity to produce less than five million. more vaccines for the rest of the world.
Meanwhile, the ACAM 2000 vaccine has strong side effects which, according to Patel, can be life-threatening for immunocompromised people.
Will we have a pandemic?
When the smallpox outbreak began, scientists argued that it was unlikely to become a pandemic. Mainly because transmission is more difficult than other diseases, such as covid-19, and because it is a known disease.

However, experts recently said the outbreak could turn into a major emergency.
In a column published in the Washington Post, Patel, along with former Harvard professor Eric Feigl-Ding and founder of the New England Complex Systems Institute, Yaneer Bar-Yam, said that monkeypox is already a “pandemic.”
His assessment is that the disease is not contained in a single geographic space. Furthermore, there is a communitarian contagion between people who have not left their countries or communities. And some patients have been infected in an “unusual” way.
“There are infected people who have no history of sexual contact or travel. This is very important to me. We need to start talking about it,” they concluded.
– This text was originally published in https://www.bbc.com/portuguese/geral-62176214
Source: Terra
Benjamin Smith is a fashion journalist and author at Gossipify, known for his coverage of the latest fashion trends and industry insights. He writes about clothing, shoes, accessories, and runway shows, providing in-depth analysis and unique perspectives. He’s respected for his ability to spot emerging designers and trends, and for providing practical fashion advice to readers.






![Tomorrow Belongs to Us: What’s in store for Friday 17 October 2025 Episode 2055 [SPOILERS] Tomorrow Belongs to Us: What’s in store for Friday 17 October 2025 Episode 2055 [SPOILERS]](https://fr.web.img5.acsta.net/img/96/95/96957c8eef9a3bd87daf877432629ae3.jpg)

