Erythroblastosis fetalis is a disease characterized by the destruction of red blood cells in the fetus or newborn by the action of maternal antibodies. But there is a treatment.

Warning: This report contains details that may be disturbing🇧🇷
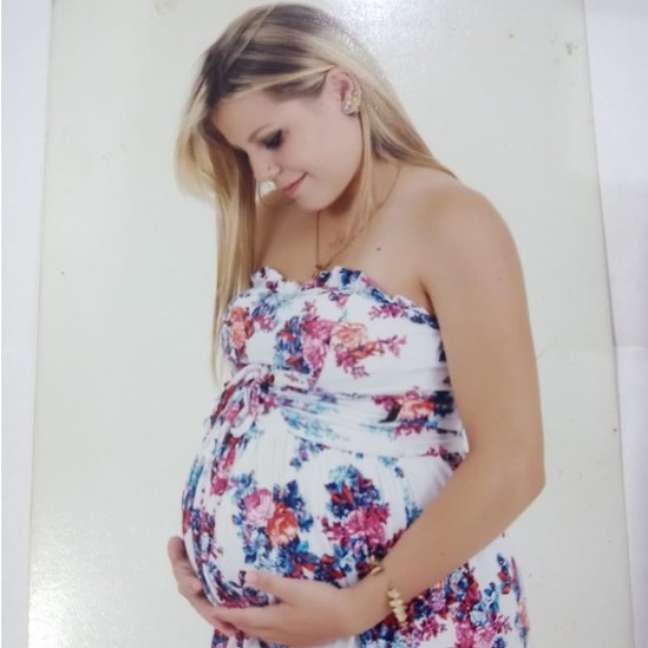
It was during her last routine prenatal visit, at 39 weeks gestation, that self-employed Karine Gehlen, 29, was told by her doctor that her baby’s heart rate was much lower than normal. For more in-depth examinations and even with the possibility of having to anticipate the birth, she Karine was instructed to go to the hospital.
After leaving the doctor’s office, the self-employed woman went to the emergency room of the public hospital in Toledo (PR), the city where she lives. Arriving there, the surprise: her child had a cardiac arrest and died.
“We did an electrocardiogram and an ultrasound and we no longer felt her little heart, it wasn’t beating anymore. At that moment my heart accelerated, I started to despair and the doctor looked at me and said: she’s dead. I didn’t know what had happened to my baby. I suggested a C-section to try and revive her, but he said nothing else would help,” she recalls.
Without knowing exactly what happened to cause a late pregnancy miscarriage, just two hours after hearing the baby’s heartbeat, Karine was hospitalized for nearly 10 hours until she had a C-section to remove the baby. .
“They put me in an isolated room because I was in total despair and sedated me so I could calm down,” he added.
It was during the hours of waiting to have a C-section that a doctor explained to Karine that she had erythroblastosis fetalis, popularly known as blood incompatibility, and that this had caused her baby to experience profound anemia, resulting in cardiorespiratory arrest.
“The doctor explained that I was RH positive and the father was probably RH negative and this difference caused my body to ‘attack’ my baby’s body. But it was very difficult to understand all this, because I had never heard of the problem , so how could I what happened?” recalls Karine.
After the caesarean section, Karine was hospitalized for another five days, unable to attend her daughter’s funeral.
Study on the subject
Dissatisfied with the loss of her baby so close to birth, having to overcome the pain of going home without her and facing the little room ready and all the clothes in order, Karine decided to better understand what had happened days before and alone to seek answers to all your doubts.
The freelancer was already the mother of a child, aged 5 at the time, and had never heard of blood incompatibility and what it could do to the child. Her first pregnancy had gone well, without incident, and her baby was born healthy in her arms.
Full of doubts, she started researching the matter, looking for explanations and solutions, as the dream of having another child remained.
“I started reading up on the subject, blood composition, why it happens and how the differences might affect a pregnancy. I emailed several doctors at different hospitals around the country to clarify my concerns and did some I tried my best to give me correct information so that when I got pregnant again I could understand what the doctors were saying and also know how to question them,” says the freelancer.
I dream of having more children
Exactly one year after the loss of her daughter, Karine received confirmation of her pregnancy: she was expecting another baby girl.
“Getting pregnant was a tough decision because I really wanted to, but trying may or may not have worked and I would have lost another baby,” she says.
Due to the incompatibility of blood between mother and child, Karine had pregnancy complications in the 21st week of her pregnancy and began to seek treatment in a hospital in Ribeirão Preto, in the interior of São Paulo, since there is no c ‘they were all the support she needed, mother and daughter they needed.
In order for the baby not to have anemia and run the risk of death, blood transfusions were needed, always inside the uterus. Transfusions occurred between 21 weeks of gestation and 33 weeks of gestation.

“Six blood transfusions were performed to survive and delivery occurred at 34 weeks of gestation. Because of the risks she was still running, it was necessary for her to stay in intensive care for 50 days and only after that she could go home, ”recalls the Autonomous.
For a year, Karine had to closely monitor the baby’s health, as there was a risk of anemia that could hamper his development. Every month the girl underwent a blood test.
“After birth, the baby still has a lot of blood from the mother, so we had to follow up to see how the blood incompatibility issue was going. It took about six months for her little body to absorb all of my incompatible blood and she was only with his own,” explains the mother.
Three years after the birth of her second daughter, the surprise arrived and Karine discovered a new pregnancy, this time without planning. Even having diagnosed the blood incompatibility, the whole process of blood transfusions and intensive medical follow-up were required. Four intrauterine blood transfusions were performed.
The baby was born on December 2nd. As her sister, she too will have to stay in intensive care for a few weeks.

Notice on TikTok
To warn other women about erythroblastosis fetalis, Karine uses TikTok and shares her experiences and learnings on the subject. She has over 1 million views on her reports.
“As I had never heard of the problem, I decided to talk about the topic to see if there were more women facing the same situation as me. To my surprise, several women started coming up with the same problem and gave up get pregnant because they thought they couldn’t. it was possible to have another child or they didn’t have the courage to risk it. I’m happy to be able to spread the word because we can get to know him before we face a situation like this of loss, “he concludes.
What is erythroblastosis fetalis
Erythroblastosis fetalis is a disease characterized by the destruction of red blood cells in the fetus or newborn by the action of maternal antibodies. It happens due to the incompatibility of the blood groups of the mother and the child, being related to the incompatibility of the Rh factor (the mother has the Rh- blood protein and the Rh+ father can father a child with Rh+).
“The disease can cause fetal hemolytic anemia, fetal heart failure, hydrops and fetal death. In the long run, fetal anemia is related to cerebral palsy, deafness and delayed development of the child,” explains the doctor Alberto Borges Peixoto, a member of the Commission of Fetal Medicine in Febrasgo (Brazilian Federation of Gynecology and Obstetrics Associations).
According to experts, blood incompatibility does not cause miscarriage in early pregnancy, usually manifests itself after the 20th week. The risk increases with gestational age and with the number of pregnancies.
“One of the ways to control this anemia is through intrauterine blood transfusion until the baby reaches gestational age and delivery can take place and the disease can continue to be treated outside the uterus,” adds Dr. Rosiane Mattar, scientific coordinator of Sogesp (Association of Obstetrics and Gynecology of the State of São Paulo).
When the baby is born, he may still have jaundice – yellowish skin and mucous membranes. This coloration is due to the accumulation of bilirubin, a result of the degradation of hemoglobin with an immature liver of the newborn.
How to make the diagnosis?
Every woman should know her and her partner’s RH factor before becoming pregnant to know if it is possible that she has erythroblastosis fetalis.

If she is positive and her partner is negative, there may be fetal incompatibility with the baby. In these cases, testing for Rh antibodies using the indirect Coombs test is recommended. This test should be repeated every month during pregnancy to check for Rh antibodies.
If there is blood incompatibility between mother and baby, the woman should take anti-Rh gamma globulin, a concentrate of antibodies that fight Rh antigens. Because immunoglobulin antibodies destroy the fetus’s Rh cells, the mother will not produce Rh antibodies. This way, erythroblastosis fetalis will not develop.
– This text was published in https://www.bbc.com/portuguese/geral-63876849
🇧🇷The best content in your email for free. Choose your favorite Terra newsletter. Click here!
Source: Terra
Ben Stock is a lifestyle journalist and author at Gossipify. He writes about topics such as health, wellness, travel, food and home decor. He provides practical advice and inspiration to improve well-being, keeps readers up to date with latest lifestyle news and trends, known for his engaging writing style, in-depth analysis and unique perspectives.





-1iukdqb6yt84h.jpg)

