Bubonic plague is still widespread throughout the world, but thanks to modern antibiotics it is much easier to treat than in the past. However, the disease may have left its mark on humanity.
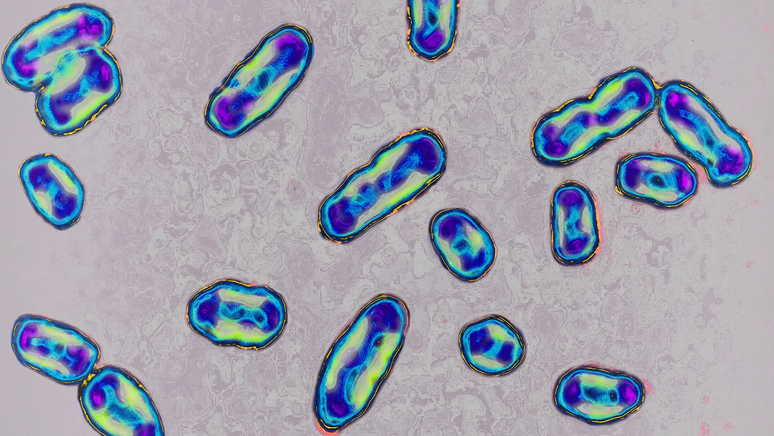
Observed under the microscope, the bacteria Yersinia pestis It doesn’t appear to be anything special.
Its shape more or less falls into bacterial standards: a kind of short stick with rounded ends. It is also relatively immobile.
But this bacterium is responsible for a disease that has exterminated a third of the European population and caused millions of deaths around the world.
Even today, the mere mention of the bubonic plague arouses fear and fascination. Currently, the disease is incredibly rare in the United States and Europe, thanks in large part to lifestyle changes that so easily prevent its transmission from infected fleas to humans.
Even when contagion occurs, bubonic plague can be treated with relative ease, using antibiotics to save people’s lives. But cases of the disease still occur.
The most recent case involves a man in the US state of Oregon who contracted bubonic plague from his pet cat. This news comes as no great surprise to evolutionary geneticist Paul Norman, who studies bubonic plague at the University of Colorado Anschutz in the United States.
“There are still small pockets of plague in the United States,” he said. It still circulates in wild animals such as squirrels and prairie dogs.
On average, approximately seven human cases of plague are reported in the United States each year. But deaths are much rarer: there were only 14 between 2000 and 2020.
The disease is more common in some parts of the world, such as Madagascar. Brazil has not recorded cases of plague among humans since 2005, according to the Ministry of Health website.
Although relatively rare compared to the past, bubonic plague has left its mark on the human species and is present in the genomes of people living today.
It is believed that the Yersinia pestis it has been infecting the human species for thousands of years. Evidence of the bacteria’s existence has been found in the DNA of skeletons dating back 4,000 years.
But in the early 1300s, a bacterial strain exploded in Europe, causing the so-called Black Death.
It is believed to have originated in the villages of the Chuy Valley in modern-day Kyrgyzstan. It may have been transmitted from infected marmot fleas to people, then spread to Europe via the Silk Road.
Estimates based on historical reports and documents estimate that the Black Death caused the deaths of approximately 50 million people in Europe by the mid-1300s.
More recent research into agricultural activity at the time (which reportedly declined dramatically, amid so many deaths) indicates that the numbers may not be so high everywhere. Some regions may have been ravaged by the disease, while others were barely affected.
It is estimated that the plague has killed at least 200 million people over the centuries.
With plague epidemics so catastrophic, researchers have long wondered whether they left any permanent mark on the human immune system.

One specific theory indicates that the plague may have spread in the 14th century to the point of creating a form of natural selection. The idea is that some of the surviving individuals were able to pass on some genetic peculiarities that would help subsequent generations.
“The Black Death put enormous pressure on the human population in Europe,” according to Norman. “It was persistent, disastrous, and anyone who had the slightest genetic advantage in that situation would have had a better chance of surviving.”
But until the relatively recent past it was almost impossible to collect any kind of data to answer this question.
DNA sequencing of skeletons of plague victims found at mass burial sites is particularly difficult. Scientists typically have to work with tiny fragments of DNA, and many of them are highly contaminated.
“It’s very common to find that most of the DNA actually comes from the soil or from bacteria that invaded the skeleton after the person died,” explains Swedish geneticist Pontus Skoglund, head of the ancient genomics laboratory at the Francis Crick Institute in London.
But experts have discovered that there is a piece of the skeleton in which intact human DNA can be reliably found. This is the bony labyrinth.
Located in the inner ear, the labyrinth is one of the densest parts of the human body. “It’s the place where DNA can be most successfully extracted,” Norman says.
“It’s a very, very small bone that remains protected in skull specimens,” he continues. “Without sounding too scary, you actually have to drill through the skull to get to that piece of bone, whereas something like leg bone is extremely porous and bacteria penetrate it much more easily.”
Over the past three years, this uniqueness has helped bring new knowledge about the people who survived plague epidemics and why.
Regulation of immunity
The human leukocyte antigen (HLA) system is made up of a group of genes that code for proteins on the surface of our cells. They play an important role in coordinating our immune reaction.
A recent study has shown that some people who were asymptomatic for Covid-19 benefited from a genetic lottery. They had certain HLA variants that served as a form of natural protection against the virus.
“The role of HLA genes is to identify foreign invasions in the body and guide the immune system to seek out cells infected with pathogenic proteins and destroy them,” explains Norman.
“Relatively rare variants of these genes may help some people survive a pandemic. If Covid deaths had been much higher, the human population today would have a much higher frequency of these variants.”
In 2021, Norman and his colleagues showed that HLA variants likely helped determine who survived medieval plague epidemics.
Researchers investigated a mass grave of 16th-century plague victims in the German town of Ellwangen. They sequenced the genomes of 36 skeletons.
Comparing them with the DNA of people living in Ellwangen today, they found that 21st-century residents have subtle differences in several HLA genes, which likely made their ancestors better able to fight off the disease. Yersinia pestis.
Two years ago, an international group of researchers attempted to examine what the impacts of the Black Death might have been on human immunity. They collected genetic samples from the skeletons of around 500 people in cemeteries in London and Denmark who died before, during and after the 14th-century pandemic.
They looked specifically at patterns for a gene called ERAP2, which codes for a protein known to help human immune cells fight disease. Yersinia pestis and other pathogens.
But one variant of ERAP2 produces a more limited form of the protein, while another generates a full-sized protein.
The study showed that medieval-era Londoners and Danes who carried the latter variant of ERAP2 were twice as likely to survive the plague. The researchers found that by the end of the 14th century, 50% of Londoners and 70% of Danes surveyed had this variant.
But we still need to know more.
Skoglund says researchers need to study thousands of other genomes of individuals who lived in Europe at the time of the Black Death and in subsequent centuries, to see whether adaptations like the ERAP2 variant were actually disseminated and integrated into our DNA.
“Any genes that had a protective effect against this outbreak could become much more frequent after the event,” he says. “But it may have only lasted a few generations.”

Skoglund even wonders whether diseases like smallpox could have had a greater impact on the formation of the modern human immune system. Smallpox was even more persistent and virulent than the bubonic plague and killed many hundreds of millions of people.
But the bubonic plague holds a specific fascination, and we can gain valuable insights by studying its impact on our distant ancestors.
“Looking at how the plague evolved and why some strains may have been more virulent in terms of mortality is important for understanding the evolution of strains that might become problematic,” explains evolutionary biologist Hendrik Poinar of McMaster University in Ontario, Canada.
Skoglund mentions his study of plague victims found in Somerset and Cumbria in the United Kingdom. They lived about 4 thousand years ago, when Yersinia pestis it had not yet developed the ability to be transmitted by fleas.
“We can observe in the DNA that the bacteria did not have a genetic factor that allowed this transmission through the fleas,” he explains. “But its evolution has had a profound impact on human health.”
“But we can also learn from how evolution dealt with problems in the past and how it created biological mechanisms to fight these diseases thousands of years ago. This is critical, and we can use it to help us develop medicines and vaccines today.”
Read the original version of this report (in English) on the BBC Future website.
Source: Terra
Rose James is a Gossipify movie and series reviewer known for her in-depth analysis and unique perspective on the latest releases. With a background in film studies, she provides engaging and informative reviews, and keeps readers up to date with industry trends and emerging talents.