Chronic pain affects millions of people around the world. Focusing on a cerebral receiver often ignored can one day offer relief.
Pain is easy to understand until it is no longer. A finger of the wounded foot or an intertwined ankle hurts. All this makes sense because the cause is clear and the pain disappears as you recover.
What if the pain doesn’t disappear? What if even a breeze look at the fire on the skin or the leg had a burning sensation for no reason? When pain persists without a clear cause, this is what is called neuropathic pain.
We are neuroscientists who study as pain circuits over time and the spinal cord change over time. Our work focuses on the molecules that silently remodes the way the pain is felt and remembered.
We did not fully understand how neuropathic pain was different from lesions relating to lesions until we started working in a laboratory that studied it. The patients spoke of a ghost pain that persecuted them every day – invisible, inexplicable and able to disturb their lives.
These conversations have changed our focus on symptoms to mechanisms. What does this ghost pain persist and how can we intervene at a molecular level to remedy?
More than just physical pain
Neuropathic pain derives from damage or dysfunctions in the nervous system itself. The system that should detect pain becomes its source, like an fire -fighting alarm that shoots fire. Even a soft touch or a breeze can be unbearable.
Neuropathic pain not only affects the body, but also alters the brain. Chronic pain of this nature often leads to depression, anxiety, social isolation and profound sense of helplessness. Routine homework can also become unbearable.
About 10% of the US population – tens of millions of people – suffer from neuropathic pain and cases are increasing with the age of the population. Complications deriving from diabetes, cancer treatments or spinal cord injuries can lead to this condition. Despite their prevalence, doctors often ignore neuropathic pain because their biology below is little understood.

Neuropathic pain can be debilitating.
Kate Wieser/Moment via Getty Images
Neuropathic pain also has an economic cost. This condition is responsible for billions of dollars in health expenditure, lost working days and productivity loss. In search of relief, many turn to opioids, a path that, as seen in the opioid epidemic, can bring addictions with devastating consequences.
GLUD1: a discreet but crucial participant
Finding neuropathic pain treatments requires answers to various questions. Why does the nervous system fail in this way? What exactly does it reconfigure to increase the sensitivity of pain or create ghost sensations? And the most urgent: is there a way to restart the system?
This is where the work of our laboratory and the story of a receiver named Glud1 comes into play. Abbreviation of the Glutamate delta-1 receptor, this protein is usually not highlighted in the titles. Scientists have long considered glud1 a biochemical curiosity, part of the family of glutamate receptors, but without any well -known function similar to that of their relatives, which usually transmit electrical signals in the brain.
Instead, Glud1 plays a different role. It helps to organize synapses, the joints in which neurons connect. Think of him as a person responsible for the works: he does not send messages for himself, but he directs where connections are formed and how strong they are.
This organizational role is essential to model the way in which neural circuits develop and adapt, especially in the regions involved in pain and emotion. Our laboratory research suggests that Gurnus acts as a molecular architect of pain circuits, in particular in conditions such as neuropathic pain, in which these circuits work badly or reconnect abnormally. In some parts of the crucial nervous system for pain processing, such as the spinal cord and tonsils, Gilud1 can model the way people feel pain physically and emotionally.
Correct malfunction
In our work, we discover that the interruptions in the glud1 activity are related to persistent pain. The restoration of the glud1 activity can reduce pain. The question is: how does Gilud tile the experience of pain?
In our first study, we discovered that Glud1 does not work alone. It joins a protein called cerebeline-1 to form a structure that maintains constant communication between brain cells. This structure, called the Transnaptic bridge, can be compared to a strong hand -taken between two neurons. It guarantees that the signs of pain are developed and filtered correctly.
But in chronic pain, the bridge between these proteins becomes unstable and begins to collapse. The result is chaotic. Like a group conversation in which everyone speaks at the same time and nobody can be listened to clearly, the neurons begin to fail and react overly. This synaptic noise increases sensitivity to brain pain, both physically and emotionally. This suggests that Gilud1 is not only the management of signs of pain, but it can also model the way these signs are felt.
What if we could restore this broken connection?
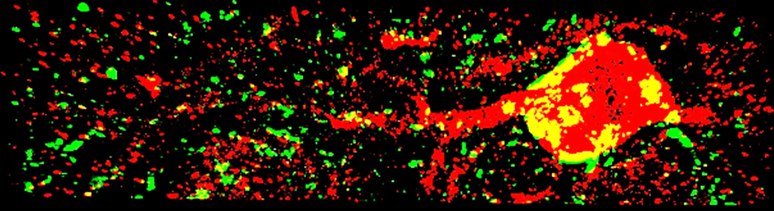
This image highlights the presence of Glud1 in green and yellow in a central amigdala neuron in red.
Pooja Shree Chettiar and Siddhesh Sabris/Dravid Lab in Texas A&M University, CC By-SA
In our second study, we inject Cerebeline-1 into the mice and we observed that it has reactivated the activity of glud1, alleviating its chronic pain without producing side effects. This helped the pain processing system to work again without the sedative effects or interruptions in other nervous signals that are common with opioids. Instead of numbing the body, the reactivation of the glud1 activity has recalibrated the way the brain elaborates the pain.
Of course, this research is still in the early stages, far from clinical studies. But the implications are exciting: GLUD1 can offer a way to repair the same pain processing network, with less side effects and less risk of dependence than current treatments.
For millions of people who live in chronic pain, this small and peculiar receiver can open the doors for a new type of relief: what heals the system, not only masks its symptoms.

The authors do not consult, work, have actions or receive funding from any company or organization that would benefit from this article and has not revealed any relevant bonds beyond their academic positions.
Source: Terra
Rose James is a Gossipify movie and series reviewer known for her in-depth analysis and unique perspective on the latest releases. With a background in film studies, she provides engaging and informative reviews, and keeps readers up to date with industry trends and emerging talents.