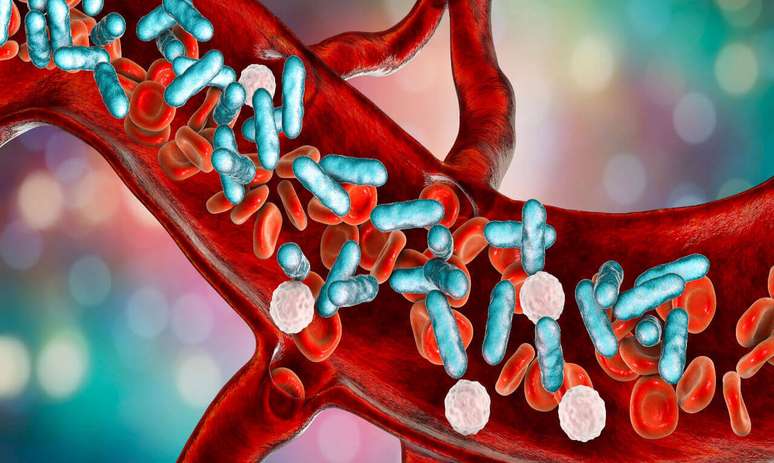
Also called septicemia or generalized infection, sepsis is the leading cause of death in intensive care units (ICUs)
OR World Sepsis Day (09/13) emerged in 2012 with the creation of the Global Sepsis Alliance. The aim of the event is to raise global awareness of this condition, also called septicemia or generalized infection.
html[data-range=”xlarge”] figure image img.img-84843aad65f62f463da3886185d5b3acjol56z67 {width: 774px; height: 463px; }HTML[data-range=”large”] figure image img.img-84843aad65f62f463da3886185d5b3acjol56z67 {width: 548px; height: 328px; }HTML[data-range=”small”] figure image img.img-84843aad65f62f463da3886185d5b3acjol56z67, html[data-range=”medium”] figure image img.img-84843aad65f62f463da3886185d5b3acjol56z67 { width: 564px; height: 337px; }HTML[data-range=”small”] .article__image-embed, html[data-range=”medium”] .article__image-embed {width: 564px; margin: 0 automatic 30px; }
According to an article published in The Lancet in 2020, with analysis data from 1990 to 2017, sepsis is the leading cause of death in intensive care units (ICU) and a leading cause of late hospital mortality, surpassing heart attack myocardium and cancer worldwide. The high mortality rate recorded globally has an alarming incidence: one person dies from sepsis worldwide every 2.8 seconds.
In Brazil, an estimated 400,000 cases occur among adults and 42,000 among children each year, of which 240,000 adults and 8,000 children die, according to the Ministry of Health, with a mortality rate among adults of 60%.
What is sepsis?
According to Dr. Arthur Faria, a doctor specialized in Intensive Medicine and responsible for the “Post ICU Rehabilitation” Care Line at the Recife Unit of the Florence Clinic, sepsis is a dysregulated response of our body to some infectious condition. The condition can be caused after infection by a virus, as in the Covid-19 pandemic, or by bacteria or even fungal infections.
“This reaction is so intense and unregulated that it causes serious damage to our body and can even lead to death. The best way to avoid and reduce the risk of contracting an infection is adequate treatment”, underlines the specialist.
Despite being the main cause of death in Intensive Care Units (ICU), sepsis also occurs outside the hospital environment. According to the doctor, serious infectious conditions can occur anywhere. “We can present a urinary infection, pneumonia or even a skin infection and, depending on the evolution and treatment, they can evolve into sepsis,” he explains.
This is because sepsis begins with an infection localized to just one organ, but soon spreads throughout the body. The doctor gives the example of a skin infection: a lesion that starts out small, then progresses to edema, increased temperature and redness at the site.
“Within a few days, some signs of a systemic reaction appear, such as fever and increased heart rate. If not treated correctly, this infectious condition can worsen with other organic dysfunctions such as drowsiness, hypoactivity, hypotension, increased heart and respiratory rate, as well as dysfunctions in specific organs, such as the kidneys, lungs, heart or liver,” explains Dr. Arthur Faria.
Warning signs
Arthur emphasizes that every infectious condition is potentially serious. The first point of attention to take into consideration is the patient’s profile. This is because immunosuppressed patients, extreme ages (newborns or elderly), people with uncontrolled chronic diseases and cancer patients, for example, tend to have a less effective immunological response and tend to have more post-sepsis sequelae, with loss of functionality. who require adequate care after discharge from hospital.
“The other point of alarm is the site of the infection. The more noble the organ, the more serious the infectious condition tends to be,” says the doctor. According to him, warning signs also include systemic response, that is, symptoms such as:
- Drowsiness;
- Mental confusion;
- Hypotension;
- Tachycardia;
- Increased heart rate;
- Reduction in the volume of diuresis (urine).
“In these cases, it is important to seek emergency service as quickly as possible. The earlier the septic condition is diagnosed and treatment begins, the better the patient’s response tends to be,” emphasizes the professional.
During the recovery phase it is necessary to keep an eye on the warning signs, i.e. the symptoms that indicate that the infectious condition is not progressing as it should. “The reappearance of fever, for example, is an alarm signal. A new clinical worsening, a worsening of the general condition, a patient who was able to have more functional independence and has lost this functionality again. In these cases, a clinical reassessment is necessary very important,” he says.
How to prevent sepsis
According to the intensive care doctor, when we talk about prevention we must divide infectious conditions into two groups: those that occur in environments outside health services, community ones and those that occur within health services.
“In the community, the main point to avoid sepsis is prevention based on broad public health measures, mainly primary care (chronic disease control, basic sanitation, vaccination campaigns, mental health, among others ).In this area, the focus is on promoting health, preventing the population from getting sick”, explains Arthur Faria.
In healthcare settings, the emphasis is on information related to patient care. “We need clear measures to reduce the number of infections in this population. Hospitals and clinics already have well-defined measures and processes designed for patient safety. The most important of these is hand hygiene, an action simple, but with a great impact in reducing infections”, underlines the doctor.
Source: Terra
Ben Stock is a lifestyle journalist and author at Gossipify. He writes about topics such as health, wellness, travel, food and home decor. He provides practical advice and inspiration to improve well-being, keeps readers up to date with latest lifestyle news and trends, known for his engaging writing style, in-depth analysis and unique perspectives.